Awareness about urinary fistula is crucial. It helps patients understand and manage its impact on their lives. Sadly, there is often a lack of education about this condition. Many people might not know much about it. This leads to stigma around urinary fistula. The condition affects communities globally but is especially prevalent in places without adequate healthcare resources. Educating oneself and others can bridge this gap, helping to create better support for those affected.
Unraveling the Complexities of Urinary Fistula
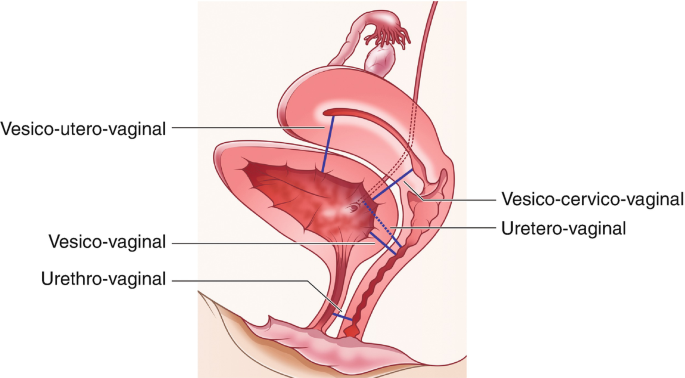
So, what is urinary fistula exactly? It’s a medical condition where there is an abnormal connection between two organs. In this case, the connection is usually between the bladder or urethra and the vagina. This often leads to involuntary urine leakage. Such conditions can sometimes be confused with other urological issues.
Urinary fistula causes vary. They can include surgical procedures, especially those involving the pelvic region. Prolonged or difficult childbirths are common culprits too, especially in rural areas with limited access to medical facilities. Another cause can be radiation therapy, a treatment sometimes used for pelvic cancers. In countries like India, the healthcare system has challenges, making it difficult to provide timely interventions. This can increase the risk of developing this condition after childbirth or surgery.
It’s important to distinguish urinary fistula from similar conditions to avoid misconceptions. Misunderstanding its origin or relating it to unhygienic practices could further stigmatize affected individuals.
Recognizing the Symptoms and Diagnosis
Knowing the urinary fistula symptoms is key. Symptoms often include continuous urine leakage from the vagina. Women may notice urine even when they’re not urinating. This is one of the most telling signs and a prompt for seeking medical advice. Persistent urinary tract infections (UTIs) are another indicator. These infections can become frequent and troubling when associated with a urinary fistula.
Early signs might also include discomfort or irritation in the vaginal area. Some women report a feeling of dampness despite attempts to stay dry. Spotting these early can lead to better management of the condition.
Once symptoms are noticed, understanding the urinary fistula diagnosis steps can guide effective treatment. Diagnosis usually begins with a simple physical exam. This helps doctors identify the issue clearly. Then, imaging techniques, such as ultrasounds or X-rays, can give a more detailed view. They help confirm the condition and its extent.
Diagnosing urinary fistula early can make a significant difference. It often leads to a better management approach and improves outcomes. Patients can then pursue the correct treatment plan and may experience fewer complications in the long run.
Treatment, Recovery, and Prevention
The urinary fistula treatment options are varied. Surgical intervention is the most common and effective method. It involves closing the abnormal connection. Surgeons are skilled in ensuring the repair is robust and sustainable.
Non-surgical treatments are options too. They are ideal for smaller fistulas or patients unfit for surgery. These methods include catheterization, which can promote healing naturally.
Beyond the treatment, the urinary fistula recovery process is crucial. Post-surgery, patients need time to rest and heal. Medical professionals guide this process, ensuring patients have the best chance for a full recovery. Regular follow-up appointments are a part of this phase, as they help monitor progress and prevent complications.
Urinary fistula complications can arise if not managed properly. Infections are a primary concern, making regular check-ups essential. Sometimes, minor recurrent fistulas might appear, requiring further intervention.
Prevention plays a pivotal role. Several urinary fistula prevention measures can be adopted. Improving childbirth conditions is vital, especially in high-risk areas. Regular prenatal care can minimize prolonged or complicated labors that lead to fistulas. For those undergoing surgery, ensuring the procedures are done in well-equipped environments can reduce the risk.
Healthcare improvements could include:
- Better access to trained medical professionals during childbirth
- Safe surgical procedures with skilled surgeons
- Availability of timely interventions in emergencies
Those at high risk should be vigilant. They must seek medical advice promptly if they suspect any symptoms. Education and awareness are critical tools in prevention, protecting future generations from facing such conditions.
Empowerment Through Knowledge and Support
Overcoming stigma requires collective effort. Education can challenge social misconceptions about urinary fistula. A well-informed community is an empowered one. Encouraging open dialogue around this condition can reduce discrimination faced by patients.
Support networks play a huge role too. Stories of individuals who benefited from community help and healthcare support inspire many others. It’s vital to connect those affected with resources and support groups. Equipping patients with knowledge and a support system strengthens their journey towards healing and acceptance.